ADVERTISEMENT INFO: SOME PRODUCTS MENTIONED IN THIS POST ARE PR (GIFTED) AND LINKS USED ARE AFFILIATE LINKS. I RECEIVED NO MONEY TO WRITE THE BLOGPOST. PLEASE READ DISCLAIMER
Thick scaly patches on your limbs, hair line and maybe even trunk that don’t go away, no matter how diligently you moisturize? This might be Psoriasis, an autoimmune disorder that affects the skin, but also many other organs and usually requires medical treatment.

But what actually is Psoriasis? Why is it dangerous, can it be cured, which skincare products are best to use to prevent flare ups and why is getting a tattoo when you have it a really bad idea?
All that and more is answered today! And if you have additional tips to share, please write them in the comments below.
What is Psoriasis?
Psoriasis is an autoimmune disease, meaning the bodies own immune system attacks parts of the body. The reason for that is, like it is for most autoimmune diseases, not yet fully understood but Psoriasis often appears together with other autoimmune diseases like Crohns Disease. It is NOT contagious.
What you see in people suffering from Psoriasis are thick, scaly patches often appearing on ellbows, hairline, knees or other body parts. They are covered in flakes that can be white, silver or pink, and are called plaques. These plaques can be anything from one to ten centimetres in size and tend to come and go, as Psoriasis is a disease that is characterized by episodes of stronger and weaker inflammatory activity. Quite often they also affect the scalp and can lead to dandruff.
There are different forms, with Psoriasis vulgaris being the most common one. There is also Psoriasis inversa that manifests in skin folds like in the groin or underneath the breasts and typically has no flakes as the environment in the skin folds is too moist, Psoriasis capitis that only affects the scalp and hair line and Psoriasis guttata. Psoriasis guttata most often manifests in children after a Streptococcus infection and is named after the small, droplet formed lesions that typically appear on the trunc.
You can also divide Psoriasis into an early onset form or Psoriasis vulgaris Typ 1, which appears before you reach the age of 40 – that one is usually the more severe form, and late onset Psoriasis or Psoriasis vulgarism Type 2, appearing after your 40th birthday, which in general is more mild.
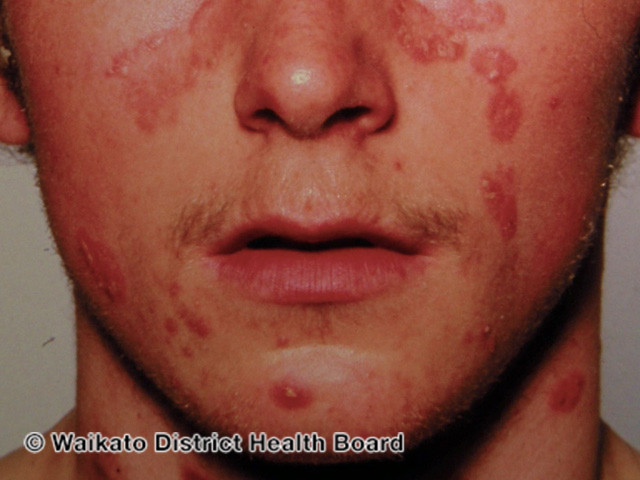
Source: DermNetNZ
Why is Psoriasis dangerous?
Now the plaques look unsightly and can be itchy and sometimes painful, but – unless they come in a massive flareup that can compromise the skin barrier to an extent where electrolyte disorders can happen – aren’t dangerous per se.
Psoriasis goes deeper than what you see on the skin though, it also affects other organs, so it comes with a higher risk for the so called metabolic syndrome, meaning the combination of elevated blood lipids, high blood pressure and diabetes and, as a result of these three, a higher risk for cardiovascular events like heart attack or stroke. Another thing it is associated with is psoriatic arthritis, an inflammation in the joints that is not only painful, but can if it goes untreated lead to disabling deformities.
So if you suspect you suffer from Psoriasis, it is really important to see a doctor for confirmation and additional treatment, even if you decide the plaques don’t bother you.

Source: DermNetNZ
What happens in the skin when you have Psoriasis?
Psoriasis is an autoimmune disease, meaning the body attacks its own structures. In the case of psoriasis, this means that so called t-cells, cells of the immune system, migrate from the blood into the dermis and release their inflammatory mediators there, things like tumor necrosis factor Alpha and interleukins.
These stimulate the basal cells to turn over around eight times as fast as they usually do, so around every 4 days and not every 28 as it would be the norm, and also travel to the skin surface much quicker. That results in skin cells reaching the upper layer of the epidermis before they have undergone the full process of maturation, which leads to them not shedding like they should, and all that means that the epidermis is around ten times thicker in affected areas than it normally is, so the skin feels thicker and that they scale instead of shedding.
On top of that the inflammation leads to angioneogenesis, meaning new blood vessels growing into the affected area, and the general redness and swelling you have with inflammation anywhere on the body.

Source: DermNetNZ
What triggers Psoriasis?
We know that, as it is with many autoimmune diseases, there is a genetic component, so if one or both of your parents suffer from Psoriasis, you are more likely to develop it yourself. Once you develop Psoriasis, there are seven major triggers that might give you a flareup. As always which one is the worst for you depends on the individual, so it is recommended you keep a journal to identify what you react most to.
These seven triggers are:
- Stress – and yes, that includes the stress of having huge scaly plaques on your forehead and not knowing if your insurance covers the necessary medication
- Streptococcus throat infection
- Trauma to the skin – that includes sun burn, scratching, rubbing, cuts and tattoos or piercings
- Weather changes – especially from warm and humid to cold and dry
- Medication – like beta blocker or Lithium for example
- Alcohol
- Smoking
You will often hear “inflammatory diet” mentioned as another trigger, but while a diet high in refined sugars and highly processed foods is never a good idea, several studies have shown that a diet specifically based around fish oils and other foods deemed anti-inflammatory doesn’t have a strong effect and should be seen as part of general preventative lifestyle changes rather than a cure. (More info: How sugar affects your skin – Glycation)
As it is very often, your hormones affect the disease as well, with high estrogen levels often leading to remission and drops in estrogen – like after ovulation, after giving birth and in perimenopause and menopause making the symptoms worse.

Image by olga volkovitskaia from Pixabay
Which skincare should I use when I suffer from Psoriasis?
Looking at the most common triggers like trauma to the skin, it is easy to understand that the skincare used when you suffer from Psoriasis should be one thing before everything else, and that is gentle. Whatever you do, avoid extra trauma to the skin, so stay clear from stripping cleansers, abrasive scrubs or dry brushing.
While plaques usually require topical prescription treatment and shouldn’t be targeted with skincare alone, things like shower oils instead of shower gels, rich fatty moisturizers, preferably without fragrance and essential oils, and salicylic acid to gently get rid of the scales are recommended and should be used even when in remission.
Your doctor might prescribe you topical steroids, Calcineurininhibitors, retinoids or creams with Vitamin D analoga to treat the plaques, and supplement with systemic medication for more severe forms and to prevent arthritis or other organs being affected.
In addition to topical treatment, there is bathing therapy where you soak in water with a high percentage of salt, and different forms of light therapy, with UVB-radiation, often in combination with Psoralen, a drug making the skin more sensitive to the sun.
You might have seen that controversial video where Kim K promoted having a tanning bed and after backlash claimed she uses it to help with her Psoriasis – there is truth to that, as UV radiation is beneficial in flareups. We know enough about the adverse effects of UV light though, namely melanoma, to use UV therapy only for a short time and very targeted on plaques, and not regularly as preventative measure.

Image by Leopictures from Pixabay
Can Psoriasis be cured?
Psoriasis is a chronic autoimmune disease, meaning it can’t be cured. Once you are diagnosed with Psoriasis, you will have to deal with it for the rest of your life. The good news is though that with medication and lifestyle adaptions, you can keep it under control.
But even when you are in remission and your skin looks and acts normal, the changes are there, dormant under the surface, waiting for a trigger that will lead to a flareup.

Source: DermNetNZ
What can I do to prevent flareups?
To prevent flareups, you need to first and foremost avoid trauma to the skin. Avoid getting sun burned, wear loose fitting clothes to avoid rubbing, don’t scratch the skin, don’t get a tattoo – I swear I am not against tattoos, it is just in this case they are really not a good idea.
Try to incorporate relaxation techniques into your life to lower stress levels, maybe consider psychotherapy to help both with stress as well as with the mental load that comes with living with a chronic disease. Exercise regularly, eat a balanced diet and try to keep a healthy weight, as being obese can aggravate your flareups – and yes, just reading all that already stresses me out. (More info: The benefits of meditation on well-aging)
On top of that, reduce your alcohol consumption as much as possible – none would be the goal, and try to quit smoking. Which is again a very hard thing to do, so if possible, try to get help with that too.
And please, go see a doctor regularly for treatment and to prevent long term damage to organs other than the skin.
TL;DR
Psoriasis is a chronic autoimmune disorder that manifests on the skin in the form of thick, red, scaly plaques, but can also affect the cardiovascular system and the joints. It is caused by immune cells of the body attacking structures in the skin, which leads to inflammation and an increase in cell turnover with insufficient shedding, which then forms these thick scaly patches you see at the surface.
Triggers are trauma to the skin, strep throat infection, stress, alcohol and smoking, so avoiding those as well as eating a balanced diet and maintaining a healthy weight will help to prevent flareups.
It can’t be cured, but treated with both topical medication as well as systemic drugs depending on the severity, and requires gentle and moisturizing skincare. While both baths in very salty water as well as light therapy are among the additional treatments, you should not frequent tanning beds for prevention, no matter what Kim Kardashian says, who is living with Psoriasis as well.
Don’t forget to check out the Discount Code Page on top if you want to save some money on your next skincare purchase.
If you want to get a vote in the next Ask Doctor Anne Topic, Ingredient Spotlight or product I review, don’t forget you can head over to my Patreon account to get more involved!